Nursing Home Staffing Star Rating
Overview
Given numerous studies point to the correlation between higher staffing levels and better patient outcomes, The Centers for Medicare and Medicaid Services (CMS) collects key performance data on skilled nursing staffing levels. Therefore, every Medicare certified long term care facility is required to submit staffing data on a routine basis. By design, CMS SNF ratings are negatively impacted by low staff levels, leading to a damaged quality of care reputation that compromises SNF referral patterns.
Stakeholders and investors in the healthcare finance sector who offer senior care lending services, skilled nursing merger and aquisition (M&A) services, operation turnaround services or nursing home valuations use CMS data to research and track KPI metrics such as staffing and staff turnover rates. Skilled nursing clinical consultants, HUD loan originators and bank underwriters use StarPRO to access CMS cost report data and care compare data to substantiate operational performance and validate the financial stability of a skilled nursing home portfolio.
Six Staffing Measures
CMS assigns Skilled Nursing Facility Staffing Star Ratings based on a facility’s performance data in six different areas. The first three measure the number of nursing hours divided by the number of residents, and the second set of three measures staff turnover. Facilities earn points in for each measure based on their staffing data metrics, then the points are totaled to determine the SNF Staffing star rating. The measures are weighted differently, meaning that there are different maximum point totals. Here’s a summary of the six measures:
- Adjusted Total Nursing Hours per Resident Day (HRD) – Max 100 Points
- Adjusted RN Nursing HRD – Max 100 Points
- Adjusted Total Nursing HRD on the Weekend – Max 50 Points
- Total SNF Turnover – Max 50 Points
- RN Turnover – Max 50 Points
- Administrator Turnover – Max 30 Points
Nursing Hours
The two major nursing categories measured are RN Staffing and Total Nurse Staffing. RN Staffing includes only hours for Registered Nurses, where Total Nurse Staffing includes hours for RNs, plus Licensed Practical Nurses (LPNs) and Certified Nurse Aides (CNAs):
- RN Staffing – Registered Nurse (RN) Hours only
- Total Nurse Staffing – RNs + LPNs + CNAs
Staffing Hours for the categories above are then divided by the number of SNF residents in the facility for a given quarter to arrive at the Hours per Resident Day (HRD), which some facilities also call Per Patient Day, or PPD. The number of SNF residents, also called Census, is determined based on patient data collected on the Minimum Data Set (MDS) assessments. For more detail on how the SNF census data is collected and used, read CMS’s documentation.
Adjustment: Going Beyond "Reported" Hours
The HRD calculated above by dividing Staffing Hours over Census is called the Reported HRD, and it represents the average number of actual skilled nursing facility hours per resident per day, as reported by the facility via PBJ.
But CMS takes staffing a step further: Staffing Star Ratings are determined based on another value called Adjusted HRD, which is calculated using the formula below:
(Reported HRD / Case-Mix HRD) * National Average HRD = Adjusted HRD
Essentially, CMS recognizes that residents have differing acuity levels that require more or less time for staff to provide proper quality of care. As a result, based on the MDS Assessments of its residents, each facility receives a Case-Mix HRD. This value is shorthand for what the expected staffing level is for a skilled facility, given the case mix, or clinical complexity, of its resident population.
CMS also releases a figure called the National Average HRD each quarter, which is an average of the Case-Mix HRDs of all 15,000+ Nursing Homes in the country, and is used in the formula to assess a given facility’s staffing levels against their peers.
So how does this all come together? Let’s look at RN hours for sample facility over a given 91-day quarter:
| Total RN Hours | = | Reported HRD |
| Total Resident Days |
| 4253 (46.74 RN Hrs/Day) | = | 0.6873 (Reported HRD) |
| 6188 (Approx 68 Residents/Day) |
Now given a Case-Mix HRD of 0.6018 and a National Average HRD of 0.3783, let’s calculate the Adjusted HRD:
With these Adjusted HRDs in hand, we can now calculate the three HRD-related measures:
- Adjusted Total Nursing Hours per Resident Day – Max 100 Points
- Adjusted RN Nursing Hours per Resident Day – Max 100 Points
- Adjusted Total Nursing Hours per Resident Day on the Weekend – Max 50 Points
Note that #3 only counts levels on the SNF weekend staffing, while the first two measure hours across the full week.
| 0.6783 Reported HRD | x | 0.3783 National Avg HRD | = | 0.4264 Adjusted HRD |
| 0.6018 Case-Mix HRD |
Want to check up on a facility's
Staffing Rating?
Let's Go Look 
PBJ & Compliance
As mentioned above, Staffing data must be submitted each quarter via Payroll-Based Journal or PBJ. Skilled nursing homes submit staffing data automatically from their payroll systems, others fill out an Excel template provided by CMS, and others use third parties to extract, compile, and submit their data. What’s key is data accuracy and completeness. CMS audits SNF PBJ data by running several compliance checks to ensure that staffing hours fall within reasonable ranges:
- No Total Nurse Staffing, both full week and weekends (0 HRD)
- Excessive Total Nurse Staffing, both full week and weekends ( > 12 HRD)
- Excessive Nurse Aid/CNA Staffing, both full week and weekends ( > 5.25 HRD)
If a facility submits data with one or more of these problems, their Staffing Rating is removed and the message “Data Not Available” is displayed prominently.
Additionally, there are other CMS data audit and data compliance checks that carry a harsher penalty — being downgraded to 1 Staffing Star:
- Failure to submit PBJ data by the deadline
- More than 4 days in the quarter without RN Staffing hours
- Failure to respond to, submit documentation for, or failure to pass a CMS audit designed to discover discrepancies in PBJ data
Needless to say, a CMS 1 star rating has an even wider impact than “Data Not Available”, so facilities need to ensure that their staffing levels are being reported in a timely and accurate fashion.
Stakeholders and investors in the healthcare finance sector who offer senior care lending services, skilled nursing mergers and aquisition (M&A) services, operation turnaround services or nursing home valuations use StarPRO to research and track CMS key performance indicators. Skilled nursing clinical consultants, HUD loan originators and underwriters use StarPRO to compare CMS cost report data and care compare data to substantiate operational performance and validate financial stability of skilled nursing home portfolios.
Turnover Calculation
The next three elements of the Staffing star rating calculation concern measures of turnover or employee retention. Studies have shown that patients receive better care when employees are happy and want to stay in their jobs. So CMS has incorporated turnover measures for both Total and RN staff, as well as a role that we haven’t looked at before — the Nursing Home Administrator. The person in this top-level, separately licensed role is singularly responsible for all the operations inside the home, so consistent leadership is key.
Turnover is more accurately described by CMS as “the percentage of staff that left the home over a 12-month period” or, in the case of Administrators, “the number of administrators that left the home over a 12-month period“.
To do this, CMS looks at the past 6 quarters of staffing history. Any employee that worked more than 120 hours within the first/oldest three quarters is included in the denominator, or pool of employees (including contract or agency staff) who are considered to be full-time. Employees who go 60 days without working in the year starting one quarter later are considered to be no longer full-time and are included in the numerator:
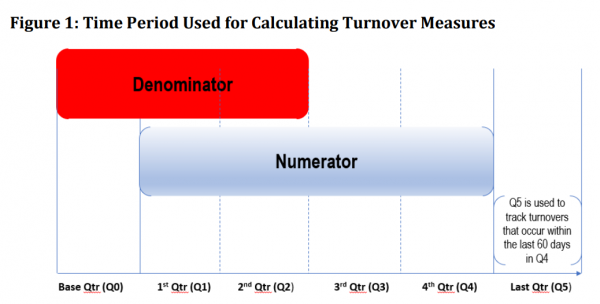
Dividing the numerator by the denominator gives us the percentage of employees who left during the year, or the turnover percent.
For Administrators, they simply check how many stopped working within the target year.
Turnover Exceptions
Because the Turnover measures require so much history, there are often issues that lead to one or more measures being excluded from the calculation of the Staffing star rating. These conditions include:
- Missing or incorrect PBJ data (see above)
- Fewer than 5 nurses in the denominator
- 100% turnover for any given quarter, which usually results from the implementation of new systems that change the Employee IDs used in the calculation
- Missing or excessive (more that 5) Administrator entries in a given quarter
The Point Calculations - Finally!
Based on national averages over a sample period, CMS established cutpoints for each of the six measures in order to determine the number of points earned. Below are the cutpoints for Adjusted Total Staffing HRD:
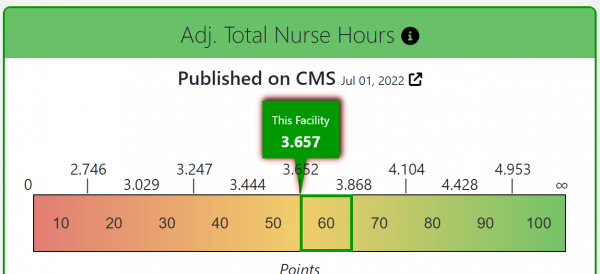
With an HRD of 3.657, the above sample home earns 60 points towards the total. Although as our screenshot shows, they’re pretty close to the cutpoint of 3.652 and need to keep those levels going up! Anyhow, this process is repeated for each of the six measures. Here’s how our sample home performed in the other measures:
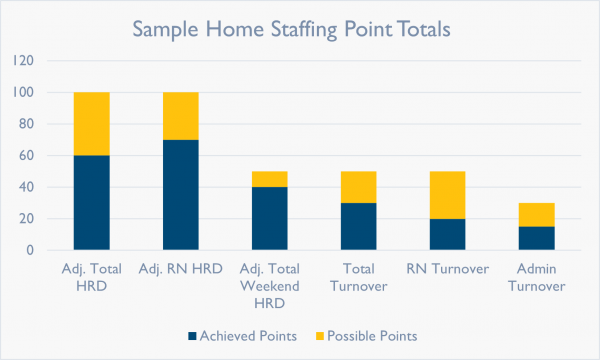
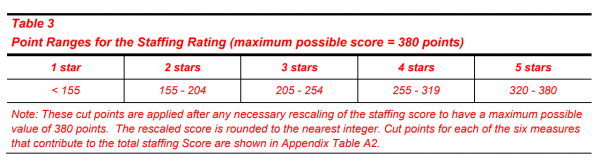
Now, the points are added together (60 + 70 + 40 + 30 + 20 + 15) and the total is compared to another set of cutpoints to determine the Staffing Star Rating. Our sample home has earned 235 out of a possible 380 points, earning them a Staffing star rating of 3.
Exceptions, Always Exceptions
All set, right? Nope. As always, there are exceptions. The issues related to the reporting of Staffing hours that we discussed will ensure that any non-compliant home is either not rated or relegated to one star, so we know that all eligible homes will have data for at least the first three measures. But so many homes have issues with their turnover data that CMS had to come up with a way to account for missing Turnover measures.
Their plan works in a way similar to the Quality star rating in that there’s an adjustment factor. So if, for example, a home has issues with its data and Administrator Turnover can’t be calculated, CMS will take the total earned points and multiply them by 380 over the total available points. Confused? Let’s revisit our sample home, minus the Administrator Turnover measure:
- Adjusted Total Nursing Hours per Resident Day – 60 out of 100 Points
- Adjusted RN Nursing Hours per Resident Day – 70 our of 100 Points
- Adjusted Total Nursing Hours per Resident Day on the Weekend – 40 out of 50 Points
- Total Nursing Turnover – 30 out of 50 Points
- RN Turnover – 20 out of 50 Points
- Administrator Turnover – Excluded
In this case, the facility has earned 220 out of a possible 350 points. In order to find the point total for their rating, we calculate 220*(380/350) = 238.85 = 239. In this case, the home is also three stars, but the missing Administrator Turnover measure was not a factor.