Fixes for the “Broken” Nursing Home Star Ratings Part 2: Staffing
05 May
Welcome to the second installment of our four-part series on how the CMS Five-Star rating system for Nursing Homes can be improved. Last month we covered the Survey domain and this month, we’re turning our focus to Staffing.
From the perspective of the operator or administrator, staffing represents a constant battle. On one hand, it’s always the most expensive line item on their income statement, and there are constant pressures to reduce spending and increase profits. On the other hand, studies confirm that high staffing levels lead to better patient outcomes and that low levels can have dire consequences. It’s hard to develop a system that strikes any kind of balance between these two interests. To that end, we think CMS deserves credit for the model they’ve created. Still, there’s always room for improvement. We think CMS can make positive change in these four areas:
- Ensuring truth through audits
- Incorporating measures of retention and turnover
- Treating larger facilities more fairly
- Addressing the LPN gap
Background: Staffing Star Rating Calculation
As a recap, the Staffing Star Rating is determined based on two components – RN and Total Nursing. The process starts with homes submitting payroll data on nursing hours in three categories: RN, LPN and CNA. The reported hours are summed for both RN alone and for a combination of all three (Total Nursing). Each is then divided by the number of residents in the building, then adjusted for patient acuity (case mix). The Adjusted Hours per Resident day (HRD or HPRD) is then used to calculate the RN Star Rating and Total Star Rating. From there, a matrix is used to match up those two ratings to arrive at the Overall Staffing Star Rating. There are also several red flags (like not having any RN hours over a weekend) that can cause a facility to be either marked “not rated”, or worse, downgraded to one star. For a more thorough explanation, see read our explainer.
Payroll-Based Journal & Audits
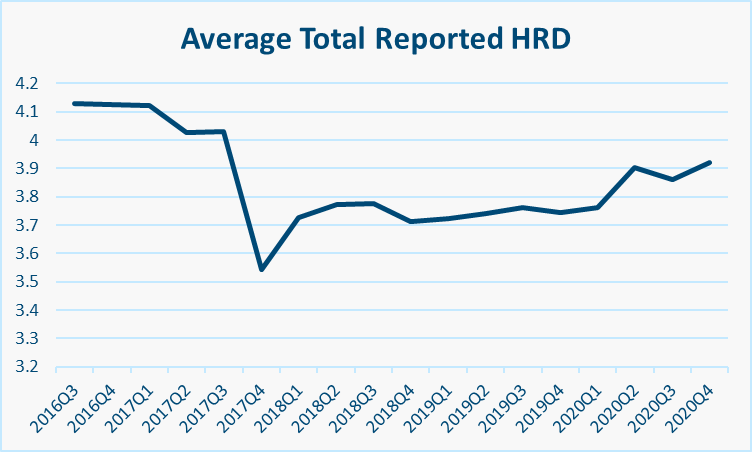
The implementation of the payroll-based system (PBJ) in 2018 was a major shift in how nursing homes reported hours. Prior to that, homes reported their hours directly on CMS form 671 and allegations of inflation were at least partially validated by a drop in HRD once PBJ was implemented. Other professionals have covered this issue well, so we’ll focus instead on how things are going now. The below charts show the Reported HRDs over time:
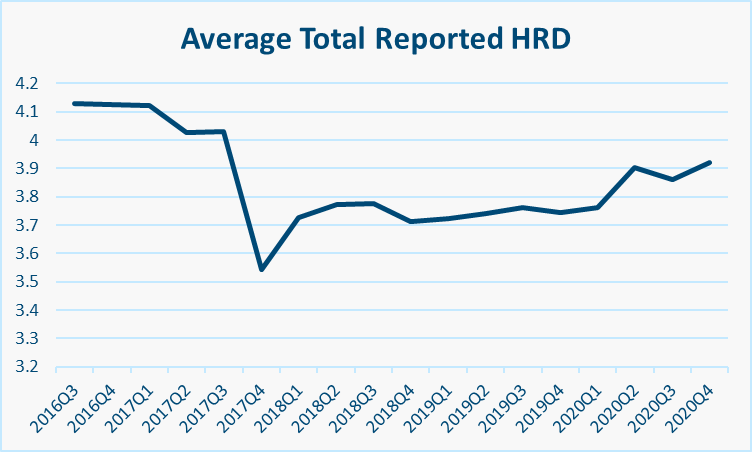

After a significant drop and subsequent readjustment post-PBJ in 2018, we see a steady climb until the onset of the pandemic in 2020, when things shoot up. Are facilities really staffing more or are they just reading the rules more carefully and getting credit for the actual hours worked? Are there unscrupulous homes finding creative ways to add hours? The recent New York Times article on the shortcomings of the Five-Star system points to one facility that included hours from nurses stationed at headquarters instead of the facility itself. Obviously we can’t verify that, but we do know that the structure of the PBJ reporting does leave some gray areas.
One such gray area is contract workers at all nursing levels, whose time isn’t always properly accounted for in a home’s payroll system. Another relates to splitting up an employee’s time across job codes, not all of which are “credit-bearing” under PBJ. How often is this detail missed? A medication aide may not spend all of their 40 hours delivering direct care, but how many facilities bother to split this up? Similarly, Directors of Nursing are often salaried positions tasked with management duties rather than direct care, but every DON we know covers for short staffing situations by checking on patients and providing direct care for at least part of their week. Do homes miss out on these hours by skipping salaried employees altogether? If we’re being honest, administrators are usually too busy worrying about a million other things to sweat the lunch break on a payroll form. This kind of minutia is part of what distracts from the actual delivery of care. We know that mistakes are probably more common than malicious intent, but inconsistencies do still exist and should be addressed.
To their credit, CMS has taken steps to do that. There are guardrails against abnormally high and low staffing levels, and they report anomalies to State Survey Agencies to use in looking for staffing issues during Survey. However, we were surprised to learn that during a yearlong audit of PBJ data, 19% of audited homes showing a significant variance in the final period of 2019Q1. CMS subsequently issued guidance to help homes avoid errors, but it’s unclear if there were any further audits. It’s our opinion that CMS could improve their reputation by conducting more audits to find these types of issues before the press does. If they’re already doing this, they should share the results openly.
Retention & Turnover
As we said above, most facilities struggle to hire, train and retain staff. The fact is that turnover is key to quality and patient outcomes. Despite a legal mandate to incorporate both turnover and tenure into the Care Compare website, CMS has yet to do so. The latest information suggests that progress has stalled as a result of the pandemic and a change of administrations. We know they’re working on it, but CMS needs to work harder and more transparently on incorporating this key measure into the Five-Star system.
Small Facilities
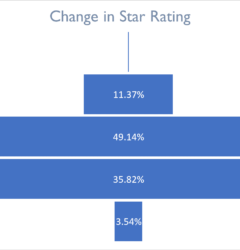
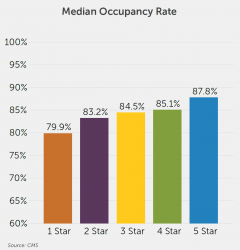
Homes with fewer beds almost always have higher Staffing Star Ratings than larger facilities.
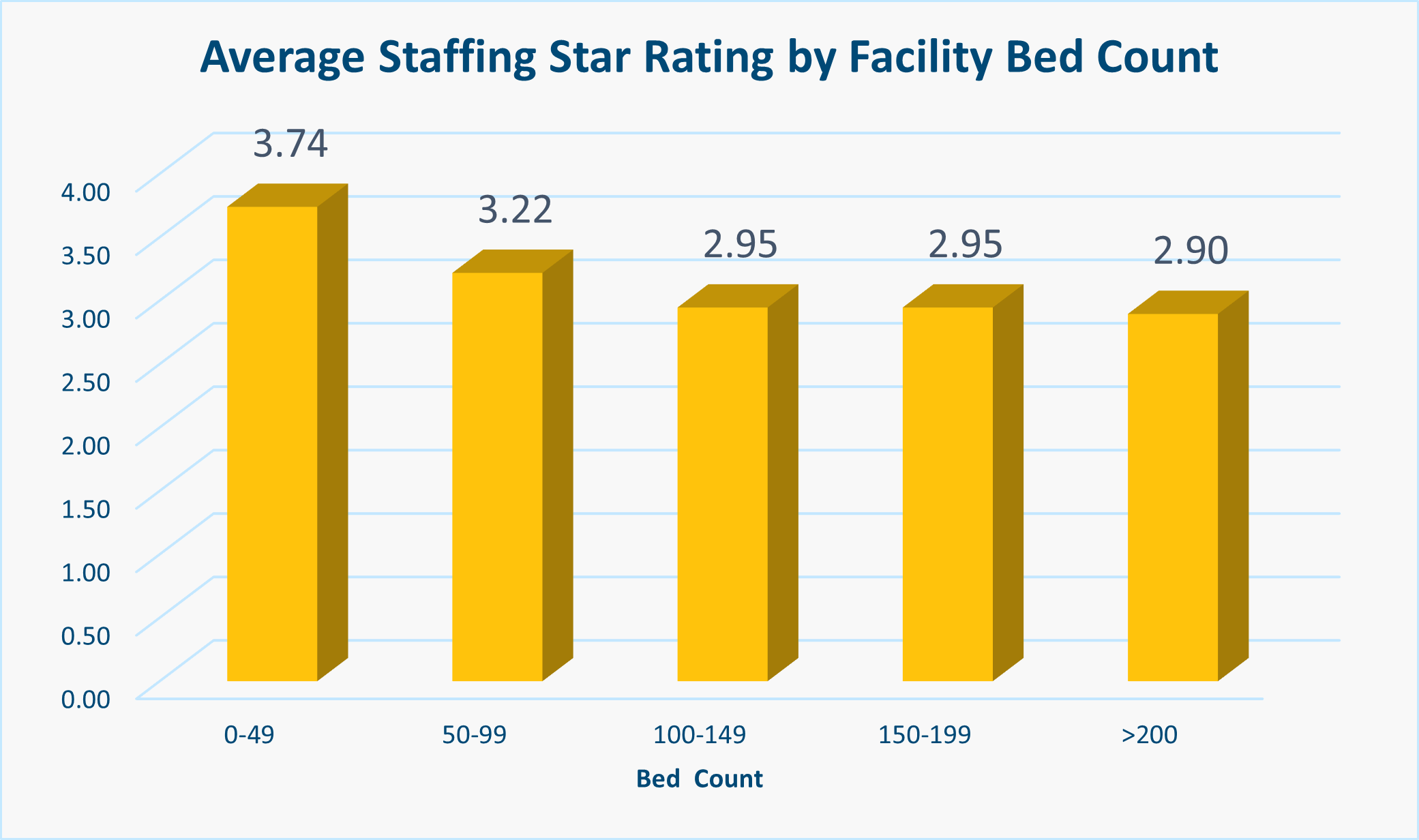
In some ways this makes sense. Teams may be more tightly knit and have better communication in smaller facilities. It’s also easier to hire and manage a nursing staff of 20 than 200. But are they really almost a full star better than their larger peers? We think the system is unfair to larger facilities who reap no rewards for efficiency or economies of scale. Residents may be getting the same level of care in both settings, but the larger home just isn’t getting the credit for it. CMS could apply a curve here to level the playing field.
LPNs – Lost in the Shuffle?
CNAs have been in the news a lot lately, and rightly so. They’re often underpaid and underappreciated, and yet their performance is key to patient satisfaction, positive clinical outcomes, and avoidance of risks from complaint inspections and lawsuits. One administrator we spoke to said that his biggest competition for CNAs now comes from unemployment, which pays more than he can afford to. Calls for improvement and better retention through higher pay and a better career path are wise and nearly universal. There are some great non-monetary solutions on hand to address these issues, but in terms of Five-Star, there’s not a need to make changes. Ditto for RNs, who by nature of their double-counting and strict mandatory minimums are well accounted for.
What we do find curious about CMS’s system is that it provides no incentive for operators to invest in LPNs. RN hours are counted both alone and as a part of the Total HRD calculation, so an investment in RNs makes sense to owners. The Total HRD calculation also includes LPN and CNA hours, but they’re counted equally. Since LPNs cost on average $10/hour more than CNAs, operators are better off cutting expensive LPN hours and making up the difference with CNAs. Obviously there are key clinical reasons why most operators don’t do this… the star ratings are important, but not that important. Still, CMS should address this blind spot. One idea is to set targets for each nursing category separately, which would also allow for separate tracking of turnover rates.
Conclusion
Our suggestions, frankly, are not unique. A recent report by the U.S. Health Department’s Office of the Inspector General outlines many of these proposed fixes and more. And states have been taking matters into their own hands more and more over the past few years: Massachusetts rejected a statewide minimum ratio, but a similar initiative passed in California, and New York just passed a budget requiring spending minimums. Despite the lofty goals set by the Biden-Harris administration, CMS is, as usual, taking its time. So, we add our voice to the chorus calling for CMS to change, and we’ll be waiting to see how they respond.
In the next installment in this series, we’ll take on the Quality domain. To be notified about that, subscribe to our newsletter below.
Related Posts
Stay In Touch
Sign up for our newsletter to get the latest updates, insights and analysis from the StarPRO team